FDA approves two sickle cell disease gene therapies, one based on CRISPR
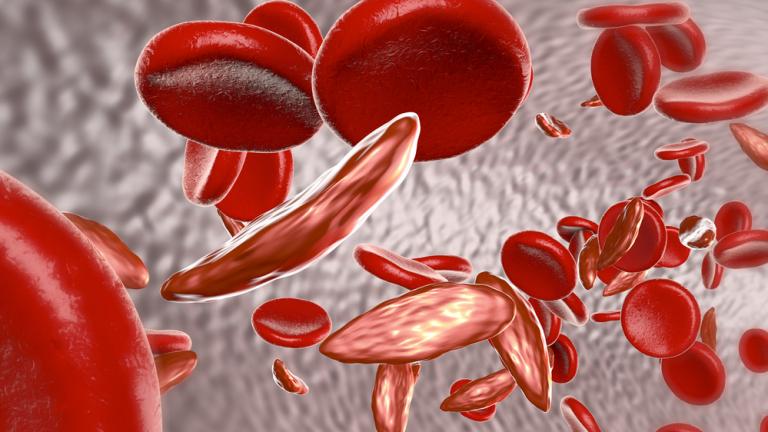
A graphic depicting both healthy and sickled blood cells. NHLBI, NIH/Handout
Dec. 30 (ZFJ) — The U.S. Food and Drug Administration approved two cell-based gene therapies, Casgevy and Lyfgenia, to treat sickle cell disease in patients 12 years and older, the agency announced on Dec. 8, 2023. Casgevy is the first FDA-approved treatment to use CRISPR/Cas9 gene-editing technology.
Sickle cell disease is a group of inherited blood disorders. It affects about 100,000 Americans, is most common in African Americans, and also affects Hispanic Americans. The disease causes a mutation in hemoglobin, a protein in red blood cells that delivers oxygen to the body’s tissues, that causes the blood cells to assume a crescent or “sickle” shape instead of being round.
Sickle red blood cells obstruct blood flow and limit oxygen delivery, resulting in severe pain and organ damage known as vaso-occlusive events (VOEs) or vaso-occlusive crises (VOCs). Recurring VOCs can be life-threatening and fatal.
So far, the only potential cure for sickle cell disease has been a bone marrow transplant, for which it is difficult to find a donor.
“Gene therapy holds the promise of delivering more targeted and effective treatments, especially for individuals with rare diseases where the current treatment options are limited,” said Nicole Verdun, M.D., director of the FDA’s Office of Therapeutics Products.
Casgevy, proper name exagamglogene autotemcel (exa-cel), requires a patient’s own CD34+ hematopoietic (blood) stem cells. These cells are edited using CRISPR/Cas9 technology at the erythroid-specific enhancer region of the BCL11A gene. The editing reduces expression of the gene in erythroid lineage cells, increasing production of fetal hemoglobin (HbF), the form of hemoglobin naturally present during fetal development. HbF binds to oxygen more strongly than adult hemoglobin, thus diluting sickle hemoglobin to a negligible amount.
Lyfgenia, proper name lovotibeglogene autotemcel (lovo-cel), uses a lentiviral vector to deliver a functional hemoglobin-producing gene. The patient’s blood stem cells are genetically modified to produce HbAT87Q, an artificial hemoglobin that has similar oxygen-binding affinity to natural hemoglobin A, also diluting sickle hemoglobin.
First, a patient undergoing treatment receives blood transfusions, minimizing the amount of circulating sickle cells. A patient must then have their blood stem cells collected and undergo myeloablative conditioning (high-dose chemotherapy for two weeks), which removes cells from bone marrow so they can be replaced. Both of these treatments then return a patient’s blood stem cells in a one-time, single-dose infusion.
Afterwards, the patient will remain in the hospital for a month for observation before returning home with three oral medications that need to be taken for three months. Yale Medicine doctors say this process is less burdensome than the existing bone marrow transplant option.
“Typically, after a bone marrow transplant, patients stay in the hospital for six weeks, they’re on immunosuppression medication for six to 12 months, and they’re taking a dozen medicines,” said Lakshmanan Krishnamurti, M.D., chief of Yale Medicine Pediatric Hematology & Oncology. “With these gene therapies, the immune system recovers much faster because they use the patients’ own cells.”
The FDA approval for Casgevy, granted to Vertex Pharmaceuticals, was based on data from ongoing studies CLIMB-121 and CLIMB-131. Results have been published in the American Society of Hematology’s Blood journals. Adult and adolescent patients with at least two protocol-defined severe VOCs during each of the two years prior to screening participated in a single-arm (no control group or placebo), multi-center trial. A total of 44 patients were treated, and 29 of 31 patients (93.5%) with sufficient follow-up time for evaluation achieved the primary efficacy outcome: no severe VOCs for at least 12 consecutive months in the 24-month follow-up period. All patients had a successful engraftment.
The most common side effects were low levels of platelets and white blood cells, mouth sores, nausea, musculoskeletal pain, abdominal pain, vomiting, febrile neutropenia (fever and low white blood cell count), headache, and itching. These side effects were from the chemotherapy, not the gene therapies, according to Yale Medicine.
The FDA approval for Lyfgenia, granted to bluebird bio, was based on a 24-month study of patients with a history of VOEs between the ages of 12 and 50 years. The relevant trials are HGB-206, HGB-205, HGB-210, and LTF-307, and results have been published in The New England Journal of Medicine. Twenty-eight of 32 patients (88%) achieved the complete resolution of VOEs between 6 and 18 months after treatment.
The most common side effects were stomatitis (mouth sores of the lips, mouth, and throat); low levels of platelets, white blood cells, and red blood cells; and febrile neutropenia, consistent with chemotherapy and underlying disease, according to the FDA.
Hematologic malignancy (blood cancer) has been observed in two patients treated with Lyfgenia, so a black box warning is prominently displayed on the treatment’s label.
The gene therapies take about a year to complete, and the high-dose chemotherapy process is “grueling,” according to Yale Medicine. The treatments will only be available at large medical centers that have the resources for advanced care.
Cost estimates currently sit at $2 to $3 million per patient. Insurance and Medicaid coverage remain undetermined.
Both gene therapies previously received priority review, orphan drug, fast track, and regenerative medicine advanced therapy designations.
References
- U.S. Food and Drug Administration - FDA Approves First Gene Therapies to Treat Patients with Sickle Cell Disease - https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease (ARCHIVE)
- CRISPR Therapeutics - Vertex and CRISPR Therapeutics Announce US FDA Approval of CASGEVY™ (exagamglogene autotemcel) for the Treatment of Sickle Cell Disease - https://ir.crisprtx.com/news-releases/news-release-details/vertex-and-crispr-therapeutics-announce-us-fda-approval (ARCHIVE)
- bluebird bio - bluebird bio Announces FDA Approval of LYFGENIA™ (lovotibeglogene autotemcel) for Patients Ages 12 and Older with Sickle Cell Disease and a History of Vaso-Occlusive Events - https://investor.bluebirdbio.com/news-releases/news-release-details/bluebird-bio-announces-fda-approval-lyfgeniatm-lovotibeglogene (ARCHIVE)
- Yale Medicine - Casgevy and Lyfgenia: Two Gene Therapies Approved for Sickle Cell Disease - https://www.yalemedicine.org/news/gene-therapies-sickle-cell-disease (ARCHIVE)
- ClinicalTrials.gov - A Safety and Efficacy Study Evaluating CTX001 in Subjects With Severe Sickle Cell Disease - https://clinicaltrials.gov/study/NCT03745287
- ClinicalTrials.gov - A Long-term Follow-up Study in Subjects Who Received CTX001 - https://clinicaltrials.gov/study/NCT04208529
- American Society of Hematology, Blood - Efficacy and Safety of a Single Dose of Exagamglogene Autotemcel for Severe Sickle Cell Disease - https://ashpublications.org/blood/article/140/Supplement%201/29/490448/Efficacy-and-Safety-of-a-Single-Dose-of (https://doi.org/10.1182/blood-2022-162353)
- ClinicalTrials.gov - A Study Evaluating the Safety and Efficacy of bb1111 in Severe Sickle Cell Disease - https://clinicaltrials.gov/study/NCT02140554
- The New England Journal of Medicine - Biologic and Clinical Efficacy of LentiGlobin for Sickle Cell Disease - https://www.nejm.org/doi/full/10.1056/NEJMoa2117175 (https://doi.org/10.1056/NEJMoa2117175)
